Matt Pfisterer was in his office at a public library in Middletown, New York, when a colleague in the second-floor children’s room called to tell him that someone was sunbathing on the lawn outside.
This sounded odd to Pfisterer, who suspected it might be a medical situation. He headed outside, bringing along a security officer. In the grass, they found a woman drifting in and out of consciousness. Ants were crawling on her shirt. They ran inside, had someone call 911 and grabbed a naloxone kit. Pfisterer remembers his hands shaking as he got the medication ready and sprayed it into her nose. About 30 seconds later, she sat up.
The timing of the episode, which took place in 2016 at the Middletown Thrall Library, was fortuitous. Just three weeks earlier, a social services provider had offered a community training in administering naloxone, a drug that rapidly reverses opioid overdoses. Pfisterer, his assistant, and multiple security guards signed up. In recent years, as the nationwide opioid crisis had hit their small community 50 miles northwest of New York City, they had found themselves calling emergency responders several times to help overdosing patrons. “Before the general news is out, people in libraries know what’s going on,” says Pfisterer, director of the Thrall Public Library District. “They’re on the street, right? They’ve got their ear to the ground.”

The opioid crisis has tightened its grip on communities across America. More than 80,000 people in the US died of overdoses involving opioids in 2022 — almost quadruple the total in 2010. In response, people like Pfisterer are equipping themselves with the overdose-reversing drug naloxone with help from local governments and community-based organizations. The approach is turning high school students, transit workers and music festival staff into de facto first responders.
Efforts are building to tackle opioid addiction before it begins, and telemedicine policies from the COVID-19 pandemic make it easier for people to get treatment. But experts say there’s still a long way to go before the crisis subsides. In the meantime, naloxone is becoming a key tool for reducing stigma and saving lives. “We all have loved ones, family members, friends who may be experiencing problems with drug use,” says Magdalena Cerdá, director of the Center for Opioid Epidemiology and Policy at New York University Grossman School of Medicine, “so having naloxone readily available to respond is important.”
The opioid crisis has been mounting since the 1990s, when millions of patients began receiving prescriptions for powerful painkillers like OxyContin that had just come on the market. Over time, some people developed substance use disorders and turned to street drugs, particularly heroin, which was often cheaper than pills. Then, around the mid-2010s, a synthetic opioid started to spread: illicit fentanyl, easier to produce than heroin and up to 50 times more potent, making it much easier for people to accidentally take too much. What’s more, because fentanyl is cheap to make, it’s often mixed into other drugs, such as heroin or cocaine, or pressed into counterfeit pills meant to look like prescription medications. Fake pills are especially dangerous for an increasing number of people self-medicating with drugs bought through social media. From mid-2019 through 2021, 84 percent of adolescent overdose deaths involved illicit fentanyl and 25 percent involved fake pills, according to the US Centers for Disease Control and Prevention. People can overdose on fentanyl without even knowing they’re taking it. This has led to a particularly dangerous moment. “The main challenge is the lethality of the drug supply that is leading to an unprecedented number of people dying from overdoses,” says Cerdá.
This is why, over the last two decades, state policies and community-level programs have worked to put naloxone within reach of people who may need it. Most states have some version of laws allowing pharmacists to provide naloxone on request without a doctor’s prescription. And in 2023, the US Food and Drug Administration approved Narcan to sell over the counter — a “big game changer,” according to Cerdá.
Naloxone can now be found in US supermarkets, convenience stores and gas stations, on shelves like ibuprofen or aspirin. People can even buy it online. That change is in addition to wide-ranging efforts to make naloxone accessible across communities. School nurses’ offices carry it. Service plazas along the turnpike in Ohio stock it. Many restaurants and bars keep naloxone on hand. Music festival-goers at Lollapalooza in Chicago were handed doses last year, and New Hampshire distributes overdose-response kits to businesses. Some cities are even placing naloxone alongside defibrillators used for cardiac arrest in public places such as libraries and community centers.
Weighed down by negative news?
Our smart, bright, weekly newsletter is the uplift you’ve been looking for.Pfisterer, the librarian, says every staff member who attended the first training with him in 2016 has administered the drug. The library had about a three-and-a-half-year stretch with no overdoses, but last winter, two people were revived. He offers training to interested staff members once a year. Since the most common type of naloxone is a nasal spray (it can also come in a syringe), it doesn’t take much time or expertise to learn how to administer it. “The more people … that are prepared to deal with an event, the safer everybody is going to be,” he says.
Still, there are barriers. Cerdá notes that people don’t always feel comfortable asking for naloxone, and many pharmacies choose not to stock it even if they’re permitted to. Plus, the cost of buying naloxone over the counter can be prohibitive for many people, Cerdá says. A two-dose kit retails for about $45 without health insurance. Still, the efforts are part of a broader push that is raising awareness and reducing stigma around naloxone, which Cerdá sees as significant. “If we normalize it,” Cerdá says, “people are much more likely to A, have it, and B, use it.”
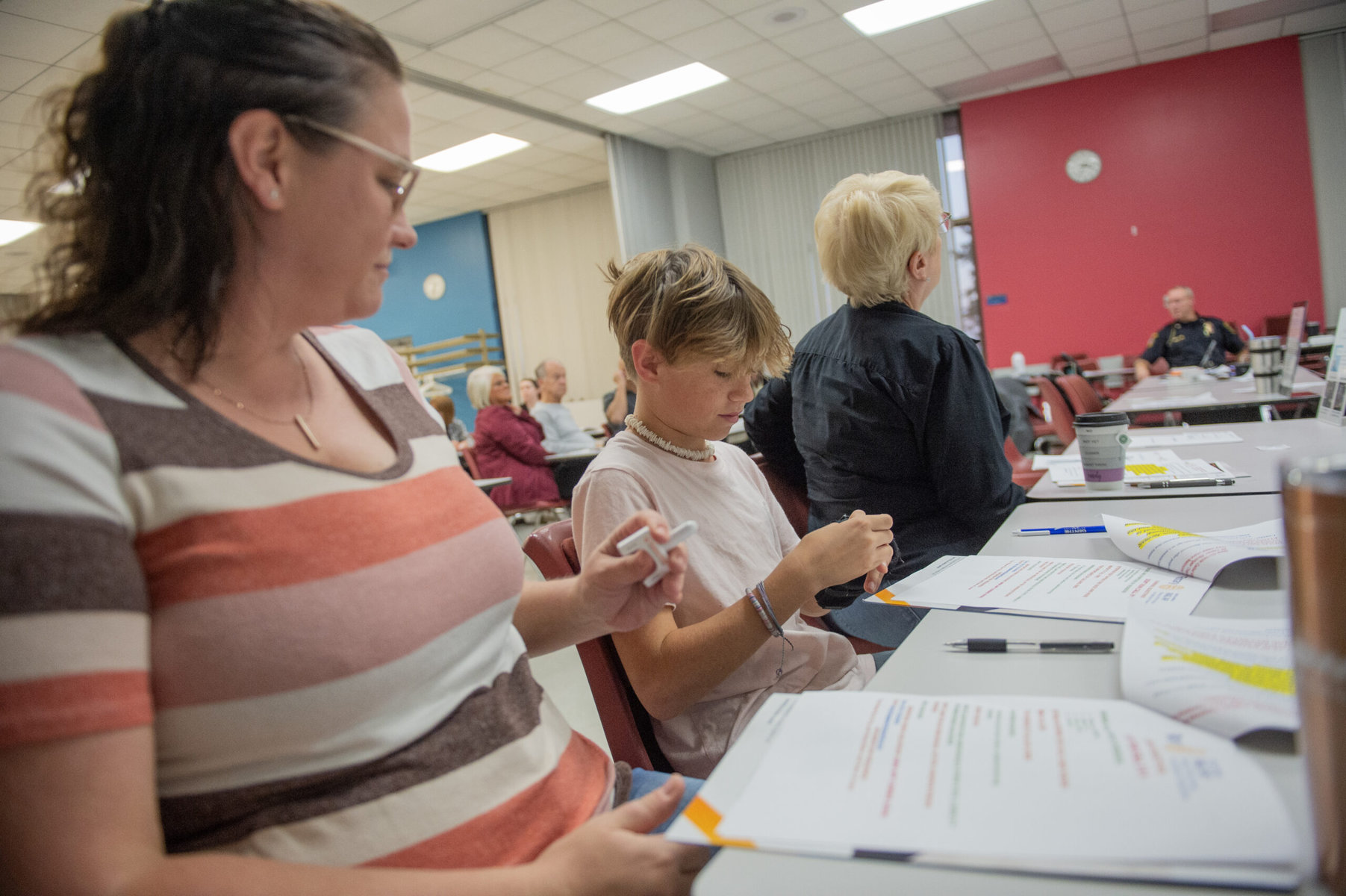
On a Wednesday evening in late June at the YMCA in Southgate, Michigan, Steve Ahles instructed a group of 14 people on what to do if they come across someone who may have overdosed on opioids. Once a person is unconscious, the retired firefighter told trainees, lay the person facing up, insert the naloxone nozzle into the nose and spray it. Then, get the person into the recovery position lying on the side, and be sure to call for emergency responders. Even if it turns out the person is not experiencing an opioid overdose, naloxone is safe to give.
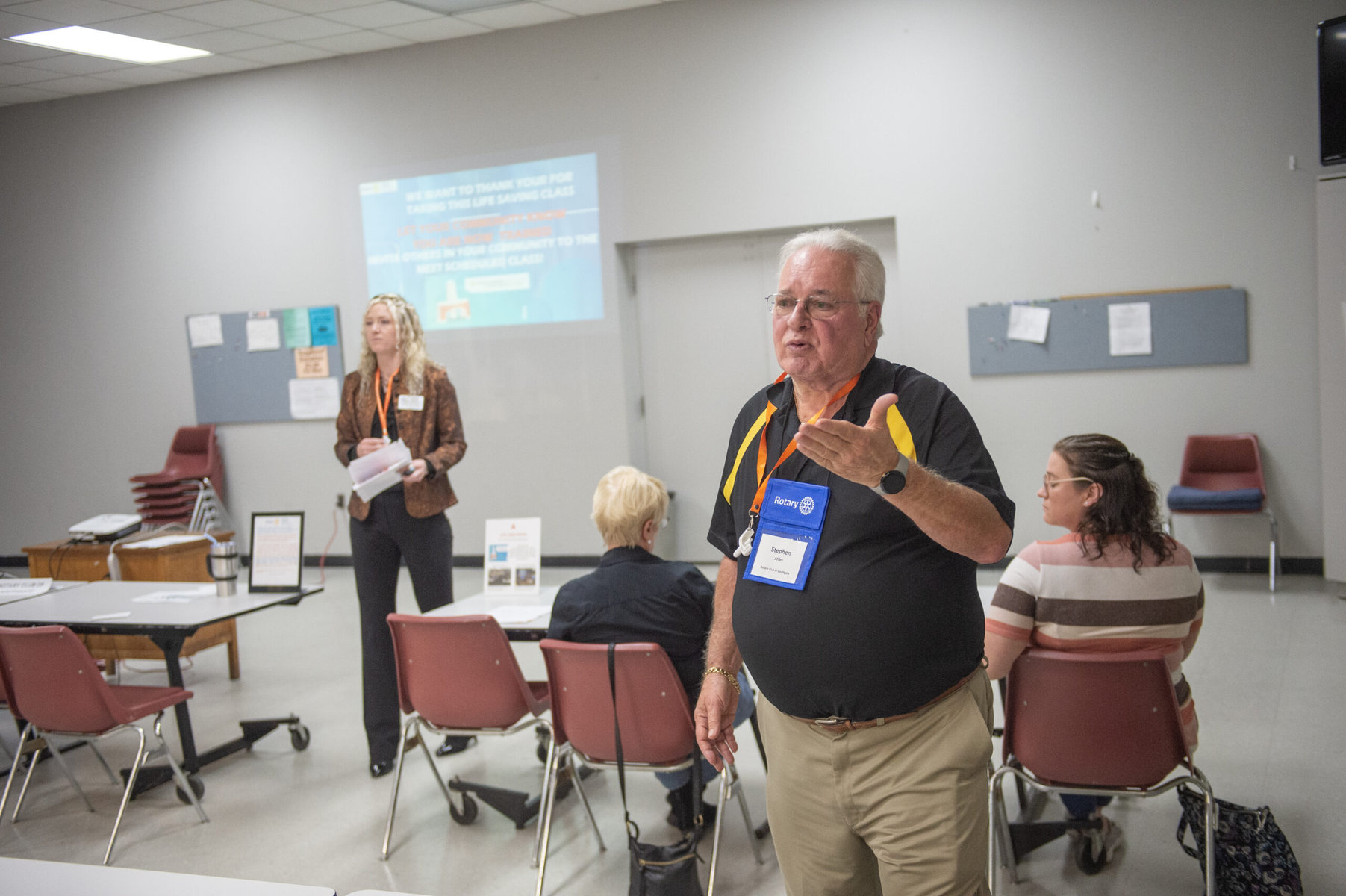
The training was the first public session Ahles had led. A member of the Rotary Club of Southgate, he had learned how to teach others to use naloxone through Project Smart, a multifaceted initiative of the Rotary Action Group for Addiction Prevention. The project mobilizes Rotary clubs in the US to address opioid overuse from prevention to treatment. Project organizers have developed programs for schools, including 30-minute age-specific education presentations and drug-free clubs for students. Another component involves distributing medication disposal kits to households, to destroy old prescriptions before they’re misused. The initiative also includes efforts to connect people with treatment options and telehealth providers that prescribe medication for opioid use disorder.
One of Project Smart’s most active initiatives so far is an effort to expand naloxone access by teaching Rotary members and others to lead training sessions in their communities. Larry Kenemore, a retired paramedic who helped launch the initiative, estimates more than 1,000 people in a dozen states have been taught how to use naloxone. People who attend are given kits to take home and asked to report in when they use one so the group can track the impact. In one recent report, a police officer in Arkansas whose department was trained through the project said he used the medicine twice, to revive a pregnant woman and a teenager, Kenemore says.
Ahles’ first trainees in Southgate included several Rotarians, YMCA staff members and a few people who found the event on social media. One woman told Ahles that one of her family members uses drugs. “It was a concern of hers that maybe this should be kept around,” he says.
As the fire chief of Southgate, Ahles was involved with an effort to distribute defibrillators in the 1990s. “I don’t see this as any different,” he says. “It’s just a tool that can help save lives that’s readily available to the public, doesn’t really require any specialized knowledge. You simply have to learn a couple of things.”

Researchers have estimated widespread distribution of naloxone to emergency personnel and other people likely to encounter an overdose could reduce overdose death rates by more than 20 percent. A study published in 2019 found that North Carolina counties where naloxone kits were passed out had lower overdose death rates than counties without distributed kits. While advocates are working to make naloxone more widely available, research shows that it’s particularly effective in the hands of people who use drugs or are likely to be bystanders. The idea is to make its public presence common, so it’s readily at hand whenever needed. “I think it’s really important for everyone, essentially, to have access to naloxone,” Cerdá says.
In a parking lot tucked behind a building on a busy street in Cincinnati, white letters glow on a vending machine 24 hours a day: “Stay safe.” Drivers can pull their cars alongside it, roll down their window, punch in a code, collect their items and drive away. The machine doesn’t offer sodas and candy bars. Instead, it’s stocked with naloxone, strips that test substances for the presence of fentanyl, safer sex kits, pregnancy tests and more.
The Cincinnati HIV-prevention organization Caracole placed the vending machine outside its office in 2021 as a mid-pandemic effort to support vulnerable residents when in-person services weren’t possible. The organization takes an approach known as harm reduction, which tries to lessen negative outcomes for people who are not ready or able to completely stop engaging in risky behavior, explains Director of Prevention Suzanne Bachmeyer.
That idea is controversial, with critics concerned that it could encourage drug use. But some elements of the strategy are being more widely embraced. Fentanyl test strips, for instance, have been considered illegal drug paraphernalia in some states. Now, they’re increasingly recognized as lifesaving tools, and at least 20 states have decriminalized them since 2018. They’re also becoming more widely available on college campuses and elsewhere amid an increase in counterfeit pills meant to resemble popular medications for everything from anxiety to attention-deficit/hyperactivity disorder.
To date, clients report that testing strips they got from Caracole’s machine have detected fentanyl in drugs about 5,800 times. And people used naloxone from the machine to reverse overdoses almost 3,500 times, according to clinical pharmacist Daniel Arendt, an assistant professor at the University of Cincinnati who partnered with Caracole to track the machine’s impact. “We found that the best bang for your buck in terms of just overall dollars spent in harm reduction is when naloxone is given to the community who is at risk,” says Arendt.
Anybody can register to get a code to access the free items in the vending machine, a process that takes a couple of minutes by phone or in person. The registration process helps track how the machine is used. But those brief conversations are also starting points for new connections, Bachmeyer explains. Many people who first interacted with Caracole through the vending machine later came to use other services, like HIV testing, prenatal care or help for domestic violence. She says multiple people have sought assistance connecting to treatment for opioid addiction.
Part of the intention of tracking Caracole’s vending machine was to learn from the experience to inform other communities, according to Arendt. Now, the organization has consulted with more than 50 public health officials and others interested in setting up similar programs. The vending machine has turned out to be more successful than organizers expected, Arendt says, though it’s no silver bullet. “This is a band-aid. This is not something that is going to solve everything,” Arendt says. “It’s something that we’re hoping will help because this current system doesn’t work well enough that these things aren’t needed.”

Carol Katz Beyer knows the opioid crisis well. Her oldest son, Bryan, died in 2016 of a fentanyl-related overdose. Four days after Bryan’s unveiling ceremony, a Jewish custom traditionally held near the anniversary of burial, his younger brother Alex also died of an overdose involving fentanyl. “The empty chairs, the holidays, the ripple effects of the loss and trying to carry on and trying to, you know, honor their legacy and their memory, because they were just the funniest, smartest, goofiest …” Beyer says, trailing off. “It’s not something a family ever forgets.”
The two brothers were always close growing up in New Jersey, Beyer recalls. They shoveled snow together, they skateboarded and snowboarded. They were a part of the same friend group and went to the same parties. And they experimented with drugs together. Once Beyer’s sons started using drugs, she says, navigating treatment options was extremely challenging. They tried out-of-state residential options. Over the course of years, the cost of treatment reached more than $500,000.
Both young men made strides, Beyer says. Bryan attended Johnson & Wales University, and Alex graduated from Full Sail University. But the road to recovery is not straightforward, and they faced stigma, strict rules and other challenges.
At times, Suboxone, a medication taken daily that can reduce symptoms of withdrawal and cravings, helped Alex in his recovery. But there were barriers that made it hard for him to continue using it. Once when he was discharged from a recovery program, he was placed in a sober living home that did not allow residents to take medications for opioid use disorder, Beyer recalls.
Beyer’s experience has made her an advocate for improving policies and treatment options related to opioids. She has led community outreach for nonprofits including Project Opioid, and through her work she’s pushed for more availability of evidence-based treatment options, including medications like the one her son used.
In the past, she explains, many people viewed medications that treat opioid addiction as trading one drug for another. But she says it’s akin to treating any other disease, like taking insulin for diabetes. “Some folks may not need or want to be on it,” Beyer says. “Other individuals may need it for a short term. Others may need it for life.”
Andrew Kolodny, medical director of the Opioid Policy Research Collaborative at Brandeis University, emphasizes that overdose deaths can be prevented by expanding access to medications that treat opioid use disorder. “To this day, one of the main policy failures is a failure to recognize that this is an epidemic of opioid addiction, an epidemic of people with a preventable, treatable disease,” he says. “If you miss that piece of it, you miss more of the upstream interventions, like prevention and treatment of opioid addiction.”
People whose treatment involves medications like buprenorphine (which is in Suboxone) and methadone are less likely to relapse or fatally overdose. “If we really want to see deaths coming down in the United States in the short run, you would want to see that everyone who’s opioid-addicted can much more easily access buprenorphine than they can heroin or fentanyl,” Kolodny says.

Dr. Arun Gupta sees the impact that medication can have on people’s recovery. The chair of Project Smart’s treatment program, Gupta has specialized in addiction medicine since 2006 and is a strong advocate of medication-assisted treatment. Eighty-five percent of his patients are stable and in long-term recovery. “They have jobs, they excel in work, they excel in education, they’re back with their families, they go to church, they buy new houses, they buy new cars,” he says.
Despite evidence demonstrating the effectiveness of medication for supporting recovery, many people don’t receive it. Nationwide, 87 percent of people with opioid use disorder are not taking medication as treatment. One of the main challenges, according to Gupta, is a shortage of physicians willing to prescribe buprenorphine. There is stigma around treating addiction, he says. Doctors also have to comply with strict regulations, putting them at legal risk if they misstep.
A federal policy change at the end of 2022 removed one barrier: Physicians are no longer required to get a waiver to prescribe buprenorphine, a shift that theoretically makes prescribing the medicine easier. Gupta is skeptical that will make a difference on its own. Treating addiction requires expertise, he says, and many doctors are unwilling to take on the issue.
Another COVID-era change has been promising. Federal regulations historically required patients to be evaluated in person to get their prescriptions. But early in the pandemic, rules were relaxed, allowing physicians to meet with patients and prescribe buprenorphine via telehealth — filling a gap in their existing treatment or giving them time to connect with a longer-term provider.
The pandemic-era rules are not permanent, and the federal rules for telehealth prescribing going forward are still being debated and revised. But research indicates telehealth leads to higher retention rates in treatment than only in-person services. Patients and doctors reported benefits like flexibility, with few downsides, and there was little evidence that the drug was more likely to be diverted and misused.
Beyer recalls that when her sons were navigating recovery, the model for addiction treatment was “tough love.” Over the years, she has seen more leaders and community members come to understand that such a punitive approach doesn’t work. Many responses are politically contentious. But there have been shifts, and with that, a cause for hope. Beyer sees more widespread agreement around the importance of medications for opioid use disorder. She’s noted a growing awareness of mental health issues, which often correlate with substance use. The crisis continues to take a toll every day. But, she says, “I like to think that as a nation, we are coming together around some of these complex issues.”
This story is a collaboration between Reasons to be Cheerful and Rotary magazine.
Photos for this story are by David Degner and Matthew Hatcher. Vending machine photos are courtesy of Caracole, Inc.



