

The Great Recovery is a series examining how a surge in innovation, outreach, access and attention to equity is improving our mental health system. It is supported by a grant from Wellcome Trust.
This is part two of a two-part story about how telehealth is bringing therapy to places where it is often difficult to access. Read part one: The World’s Therapists Are Talking to Ukraine
Suffering from dementia, 94-year-old George (not his real name) was admitted to a nursing home in a rural town in California in 2019. Since he lacked family nearby, he received few visitors. George soon became lonely and depressed — and these feelings were exacerbated by the sense that there were few people he could connect with at the home. His failing memory led to confusion and frustration, culminating in George putting a bag over his head in an attempt to end his own life last year.
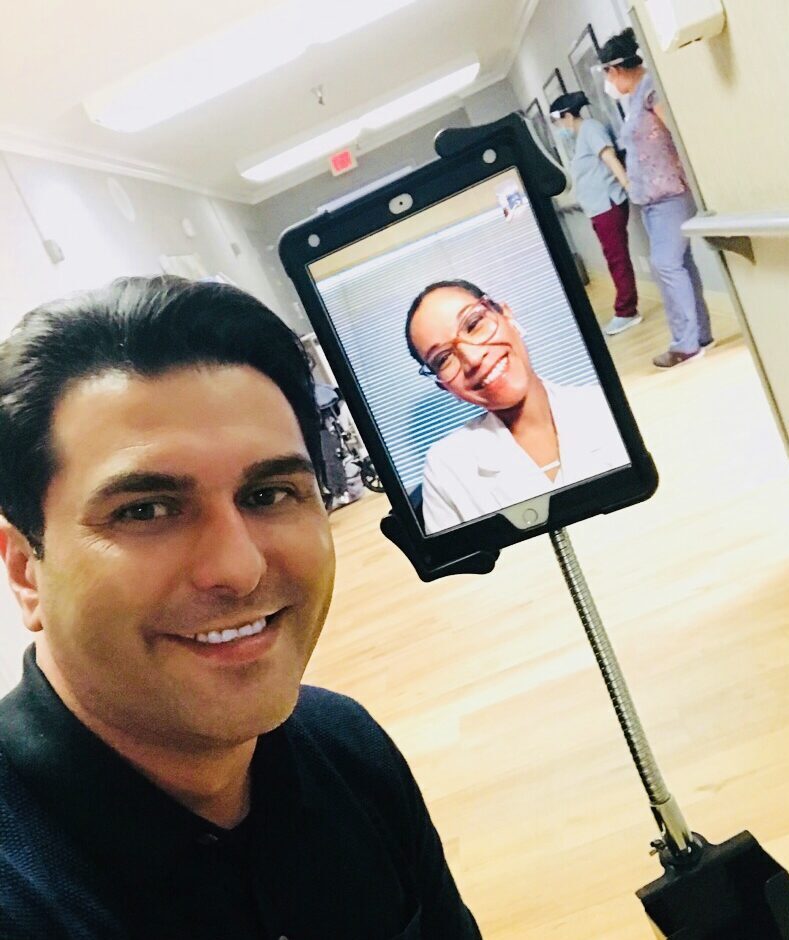
Despite the nursing home’s social services director identifying him as a candidate for psychotherapy, no psychologists were available to visit George in-person due to the home’s rural location. Instead, George was set up with a clinical psychologist who could work with him remotely in weekly telehealth psychotherapy sessions.
After his initial psychologist left the company, George began seeing Dr. Jennefer Ho, senior clinical manager at Executive Mental Health. George’s sessions have helped him process his feelings and embrace life in the facility, while also accepting his difficult relationship with his daughter, with whom he previously lived.
“Telehealth has made a huge impact on George’s life,” says Dr. Ho.
George is one of the estimated 122 million Americans, or 37 percent of the population, who live in the 5,833 federally designated “mental health professional shortage areas.” That number rises to 80 percent of the population in some states, with two-thirds of the shortage areas located in rural parts of the country.
About a fifth of Americans living in rural areas are reported to have a mental illness, according to a study published by the Journal of Clinical and Translational Science. The study also notes that, while the prevalence of mental illness is similar across rural and urban areas, there has been a significant disparity in treatment levels. In other words, rural residents like George simply don’t have access to specialist medical professionals like psychologists that are available to their urbanite counterparts.
Telehealth services have shown promise in meeting this need. In a 2021 study, rural residents reported growing acceptance of, and satisfaction with, telehealth services for a range of medical needs. Telehealth services bring overall benefits like better access to care, reduced costs to the patient and health care provider, and increased training for health care professionals — which in turn leads to better recruitment and retention.
Still, challenges remain: A 2023 study found telehealth uptake to be low in rural populations because many residents lack the required technology, such as digital devices and high-speed internet. Issues like language barriers, and visual and hearing impairments are also more likely to hinder rural residents’ use of telehealth services in general, according to a 2021 national survey conducted by the Bipartisan Policy Center and Social Sciences Research Solutions.
Weighed down by negative news?
Our smart, bright, weekly newsletter is the uplift you’ve been looking for.Progress is coming on the technology front: In June, the Biden administration announced plans to pour $42 billion into ensuring every home in America can access high-speed broadband by 2030. Meanwhile, providers like Executive Mental Health are doing their part by equipping partner nursing homes with a tablet, with teleconferencing software already installed so residents can easily access their sessions. They also provide an on-site assistant to supervise appointments and sterilize equipment between sessions.

For those with dementia, like George, the goals of the sessions range from monitoring behavioral issues and possible psychotic symptoms to helping patients process the difficulty of their own declining cognitive functions, explains Dr. Ho. Sessions sometimes consist of what she calls “reminiscence therapy” to validate what a patient has accomplished throughout their life and make meaning of their experiences.
“Often, patients with dementia complain about the regrets that they live with. The goal of psychotherapy in that case would be to teach them self-compassion so that they can accept the decisions they’ve made in life, and to stop mentally beating themselves up over past mistakes,” Dr Ho adds.
Jen Amis, president of Encounter Telehealth (which has partnered with around 200 nursing homes and assisted living centers, the majority in rural areas) says a telehealth consultation is often the first time a resident has ever received mental health support. It’s also a much more convenient alternative to what can commonly be a four-hour round-trip for a one-hour appointment, accompanied by two staff members, in a wheelchair-friendly vehicle if required.

Beyond that, telehealth is a more effective form of treatment than visiting a local primary care provider, which can result in over-prescription — specifically in antipsychotics medication, to treat the aggressive behavior that often accompanies conditions like Alzheimer’s or dementia.
“Antipsychotics are really powerful drugs, and should really only be prescribed for people with schizophrenia or bipolar disorder, who need that. But I call it the ‘drool’ effect, because that’s what it’s doing,” says Amis.
Indeed, Encounter Telehealth’s Antipsychotic Drug Reduction Study released this year noted that elderly patients with dementia who are treated with antipsychotics don’t see an improvement in their functionality or quality of life, and are at an increased risk of death. Falls are more likely, as side effects of antipsychotics can include sedation, vision issues, and weakness and/or stiffness of the muscles.
Amis says Encounter Telehealth sees a significant reduction in antipsychotic prescription rates when they start working with a nursing home that did not previously have specialized behavioral health care. Encounter’s analysis showed that, in 2022, its nursing home partners prescribed antipsychotics at rates 7.5 percent below state averages and 4.1 percent below the national average.
“When we go in, the first thing we’re looking at are those antipsychotic prescriptions — to reduce and hopefully eliminate them, to get the number of pills that they have to pop everyday down,” says Amis. “We’ve got letters from adult children saying they just had the first conversation with their mom in over a year, because we’ve done that.”
Recognizing the collaborative effort it takes to support individuals in need, Encounter Telehealth also provides its services to families of its nursing home residents, as well as staff.
“If your parent is in a nursing home and has a diagnosis of dementia, you can meet with our provider to help talk about what to expect with progression of the disease, how best to communicate with your loved one and what behaviors you might experience,” says Amis. “It’s a complicated time for everyone involved.”
“If we can help manage the progression of that illness peacefully, then it has a wider impact on the whole community, not just that person and that person’s loved ones, but the other residents in the facility, and even the staff.”
For George, thanks to regular telehealth sessions, he’s begun engaging more in activities in the nursing home and making more effort to visit friends who also reside in the home.
“We have worked on acceptance of his relationship issues with his daughter, but also focused on valuing the relationships that he does have in his life, such as with nurses and other residents,” says Dr. Ho.
Moreover, despite his dementia, Dr. Ho says George’s appreciation for the care is clear. “George always tells me and my assistant how much he looks forward to seeing us on a weekly basis,” she says. “Despite his memory impairments, he always remembers who we are.”





