This story originally appeared in Rotary magazine, the official publication of Rotary International, a service organization with 1.4 million members around the world. For more information, visit Rotary.org.
Carol Rosenstein was watching her husband, Irwin, slip away inch by inch. At one time he had been a brilliant lawyer, a lover of Broadway musicals, a world traveler. But after his diagnosis of Parkinson’s disease in 2006, he developed dementia, and slowly everything changed. His gait flattened to a shuffle. The sparkle in his eyes turned into a blank stare. His mood soured. Worsening matters, the medications he took caused hallucinations and extreme agitation. As communication grew more challenging, Carol felt the distance between them growing.

Then, in 2014, something happened. Irwin, who had been a gifted pianist since childhood, sat down at the piano and began to play. As his fingers floated through American classics like “Fly Me to the Moon,” “What a Wonderful World,” and “Try to Remember,” Carol saw his posture straighten. The sparkle returned to his eyes. The husband she once knew came back, bit by bit, if only briefly. “I could see this human being resurrect and start to reconnect with his environment,” she says, “just like I had given him a dose of medication.”
Mystified, she called his neurologist and asked what was happening. “He said, ‘Carol, you are watching the power of music, changing brain chemistry.’”
That statement would go on to change not only their lives but the lives of countless others.
Music, it turns out, is medicine for the mind.
While it’s tempting to search for a woo-woo reason why music resonates with us so deeply, it’s not necessary. For people like Concetta Tomaino, the effects can be explained by science and logic — even if there’s still a lot to learn. “I think I went past that magical, mysterious piece a long time ago,” she laughs. Tomaino is one of the pioneers in this area; she has been researching how music affects all aspects of neurologic function for more than 40 years. To her, the impact of music on the mind and body demonstrates how much of our makeup as human beings is based on rhythm, resonance, and perception, all of which connect us in a fundamental way to who we are. “Everything in the world is a vibration of some kind,” she says. “Music is an extension of who we are, and that’s why it helps us reach people who seem to be disconnected because of illness or a traumatic brain injury.”
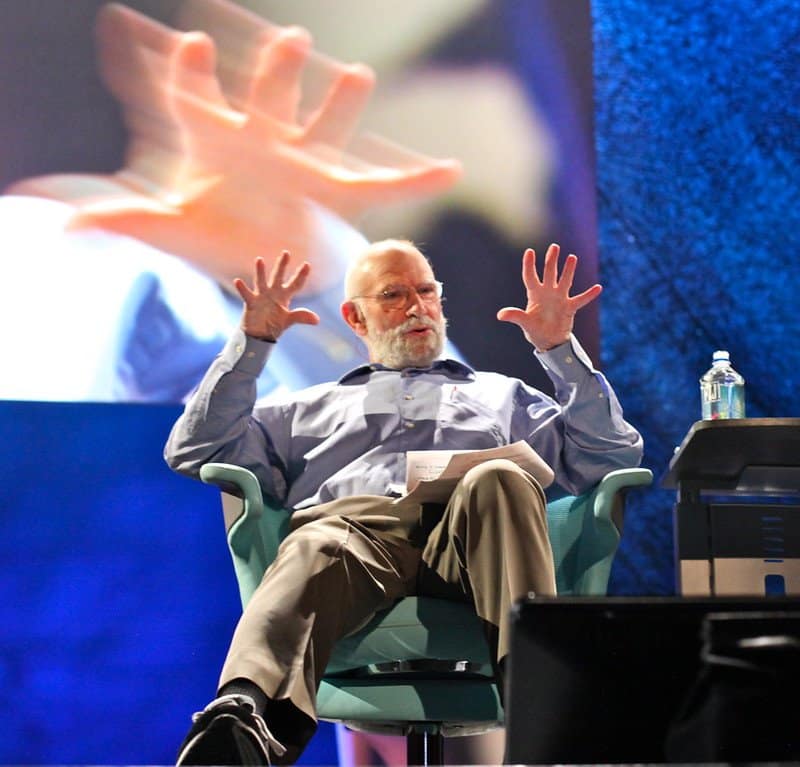
Tomaino spent decades as a music therapist, pursuing evidence-based research around music and the brain before volumes of such literature existed. In 1980, she began working at Beth Abraham Hospital (now Beth Abraham Center) in the Bronx, New York, where she first met the consulting neurologist Oliver Sacks. By then Sacks had already written Awakenings, an autobiographical book (and later a movie) about a group of encephalitis lethargica patients frozen in trancelike states, whom he “awakened” using a new drug, along with music.
Like Tomaino, Sacks was extremely interested in understanding more about the potential impact of music on patients. In 1995, the two co-founded the Institute for Music and Neurologic Function, where Tomaino remains the executive director, to better understand the ways that music helps people with neurological problems to move better and remember more.
Sacks, a legend who wrote many books on his patients’ neurological experiences, including Musicophilia, which delves into the effects of music, passed away in 2015. His words on the topic remain as evocative and poetic today as when he spoke them in 1991 before the U.S. Senate’s Special Committee on Aging: “Though the nervous system is sometimes compared to a computer, I think it is much more like an orchestra or a symphony. I think we are musical through and through, from the lowest levels of rhythm in our nerve cells to the highest levels. There is a vast range of neurological disorders in which this inner music is impaired, and all of these can be transformed by the healing power of music.”
Music has a way of worming into the brain, whether it’s jingles you can’t forget or songs that really resonate. They’re tied to strong, emotional moments and experiences in your own autobiography. And they’re not just stored in one area of the brain. Rather, Tomaino says they’re ingrained in the more fundamental mechanisms of brain processing. In other words, the music that we love actually becomes a part of who we are.
Because of that, when we hear those old, meaningful tunes even a half-century later, they stimulate multiple areas and networks of the brain — including areas that are relatively unharmed by a disease like dementia — and those long-ago memories resurface. That’s why a person with memory impairment may not recall their daughter’s name but may remember all the lyrics to her favorite lullaby. “It’s pulling from emotions, it’s pulling from feelings, it’s pulling from interpersonal associations, it’s pulling from a date or time or period of one’s life — historical things,” Tomaino says. Music serves as a clue, coaxing the brain to fill in the blanks.
After her call with the neurologist, Carol Rosenstein began to wonder: If music could help her husband return to himself, even briefly, what could it do for others? She grabbed her Rolodex, told Irwin’s story to her friends in L.A., and invited other “like-minded” people to a night of making music together at a studio space in a private school.
About 30 people showed up. While most of them made small talk, Irwin and three other men, all of whom had neurological conditions, made a beeline for different instruments. A man with Parkinson’s sat at the drums. Another, with Alzheimer’s, settled in at the piano. A third, who no longer spoke, pulled a harmonica out of the breast pocket of his jacket. Irwin gravitated toward the saxophone, an instrument he had played in his college marching band. They didn’t converse, and they didn’t need to. As they started to play, music became their shared language.
“These four strangers became like soulmates in a sandbox,” Carol recalls. “Instead of buckets, shovels, and spades, they had musical instruments, and this was their second childhood. They found each other, they used the music, they bonded.”
Carol was so eager to keep the quartet’s energy going that she formed a band, called The 5th Dementia, and launched a nonprofit called Music Mends Minds. The band’s “core four” grew to more than two dozen members and met regularly at Brentwood Presbyterian Church. Local and then national media got wind of it, and, in 2015, a story about The 5th Dementia aired on PBS NewsHour.
Since its humble beginnings in 2014, Music Mends Minds has expanded with more than 20 bands around the globe. (Most of the bands are now meeting virtually because of the pandemic, and are led by a music therapist.) In 2018, CNN named Carol one of its CNN Heroes.

Carol Rosenstein saw more and more scenes that reinforced the power of music: people who couldn’t remember their own names crooning Frank Sinatra; men and women who barely talked, playing instruments; older adults pushing aside their walkers to dance. She also learned more about the science behind it, thanks to such academics as Michael Thaut, a professor of music and neuroscience at the University of Toronto who is now on the advisory board of Music Mends Minds. Thaut has been researching how music affects the brains of people with Alzheimer’s in hopes of pinpointing ways to improve their lives. He says that scientists aren’t sure what causes Alzheimer’s, which is the most common type of dementia, and that while medications may treat some symptoms, there is no cure.
When a person has Alzheimer’s, the proteins in their brain don’t function normally, and that leads to the death of brain cells. A person in the early stages of Alzheimer’s may forget words or repeat questions. In the end stages, they may experience delusions and forget how to do even the most basic tasks, like eating or walking. According to the U.S. Centers for Disease Control and Prevention, as many as 5.8 million Americans have Alzheimer’s. By 2060, that number is expected to nearly triple.
In a study published in the Journal of Alzheimer’s Disease in 2021, Thaut and other researchers set out to see what happens in the brain when a person with mild cognitive impairment or early Alzheimer’s disease listens to their favorite playlist for an hour every day for three weeks. At the beginning and end of the study, the 14 participants had brain scans and took neuropsychological tests that involved memory exercises.
To Thaut’s surprise, at the end of the trial the participants showed a small but statistically significant improvement in memory — something that is extremely unusual in people with Alzheimer’s or any type of dementia. Close examination of the brain scans revealed visible changes. Most notably, Thaut saw that measurable new connections had formed between different regions of the brain — highways, if you will, that actually changed brain plasticity and also improved function in relaying information. Thaut says the research shows that while music is in no way a cure for Alzheimer’s, it can provide a “cognitive boost.”
But not all music has the same impact. In another study published in 2020, Thaut and his colleagues compared brain activation when study participants listened to two different types of music: music that dated back at least 25 years, and music that was new to them. What they found was that the different types of music activated different parts of the brain. With new music, brain activity appears limited to mostly auditory processing, but not deep processing. Familiar music, however, stimulated more regions more significantly in a way that is deeply encoded in the brain. Those regions are associated with emotion, cognition, and autobiographical memory, and are minimally affected by early-stage Alzheimer’s. “This is one of the reasons, possibly, that some musical memories are preserved, because they’re encoded in such widely distributed regions,” Thaut says. “So the chance that some of the regions associated with music-based memories are preserved is just higher.”
While the “why” of it all isn’t yet fully known, Thaut says that mood and memory are closely connected, and networks of memories can become connected to mood “nodes.” He describes it as a kind of classical conditioning: You hear a certain song that was important in your past and you automatically think of a certain time or event connected to the music. When you listen to that music more frequently, it’s like a cognitive workout for the brain. “When you drive these networks on a regular basis,” Thaut says, “you exercise those networks, and then the connectivity within these networks becomes stronger again.”
When those who live with and care for people with diseases such as Alzheimer’s and Parkinson’s seek out music and musical groups to help their loved ones, they often find the experience benefits them, too. And there’s research to support that.
For decades, Mary Mittelman, an epidemiologist who works at New York University as a researcher in the department of psychiatry, has been developing and studying social and psychological methods to help people with cognitive impairment and their family members. In 2011, curious about the impact of music, she started her own chorus, called The Unforgettables, to investigate what rehearsing and performing in a concert could do for participants. The initial chorus consisted of 22 people — 11 had memory impairment and 11 were their family caregivers. Mittelman’s published findings documented improvements in quality of life and communication not just for those with memory impairment but also for caregivers, who reported improved social support and self-esteem thanks to the chorus.
Anecdotes shared by the choral conductors stand out in Mittelman’s report. They saw couples holding hands and looking into each other’s eyes, “as though they were first dating.” They would joke around. Song lyrics would bring back memories and spark conversations. Beyond those observations, Mittelman remembers watching transformations among participants: Some would arrive grunting, agitated. They would leave speaking in full sentences, calm.
Irwin Rosenstein passed away in January 2021, 15 years after his diagnosis and seven years after rediscovering music. In those final days, Carol recalls, he could no longer speak and could not leave his bed or a wheelchair. His smile was a memory. He would look at his wife with a gaze that she refers to as the “Parkinson’s stare.”
Unless, that is, there was music.
All the way until the end, Carol made rhythm a part of their lives. As Irwin lay in bed, she would pick up two little egg-shaped shakers and play music and dance in front of him. “He was like a corpse under his blankets. Then his arms would start to come out of the covers, his knees would start to lift, and before you knew it, he was dancing with me,” she says, smiling through her tears. “That’s how we said goodbye, because his brain was so connected to the rhythm of the music when everything else was gone.”
Music could bring Irwin back to the moment, back to himself. It also brought him back to Carol. “It is painful to watch your beloved slip away inch by inch,” she says. “And if it weren’t for the music, I wouldn’t be sitting here today. As a caregiver and first responder, I can tell you, I would have never survived the journey.”


