This article was original published in Shelterforce.
Rest. Heal. Recover.
To people with serious illnesses and injuries who are also experiencing homelessness, those three words seem impossible to achieve. How can one rest when lying on a blanket in public is considered a quality-of-life infraction? Where can one heal or recover when medicine and other personal belongings could be thrown away without a moment’s notice?
Over the last decade, medical respite care programs have been bridging the gap between housing and health care for people experiencing homelessness. These programs provide private space for unhoused folks who are too ill to recover from an illness or injury on the streets, but do not require hospital-level treatment.
Since 2012, medical respite programs have more than tripled in the US, from 43 to more than 145 as of May 2023, according to the National Institute for Medical Respite Care (NIMRC). These programs — typically offered in freestanding facilities, homeless shelters and even motels — exist in 40 states, spanning Washington to Maine and as far south as Georgia and Florida.

Medical respite programs could play a key role in closing the health care to homelessness pipeline, says Devora Keller, the director of clinical quality improvement at the National Health Care for the Homeless Council. This pipeline refers to situations when an unhoused individual is discharged from a hospital back to the streets after receiving care, instead of being sent to a shelter or supportive housing unit.
Hospitals have done a lot of work to address gaps in discharge policies that allow people to leave their care without a place to live, Keller says. This means that some hospitals now require that a person experiencing homelessness be discharged to a living facility. But there aren’t enough shelters that can provide resources for people who need additional help treating an illness or injury.
“We live in a country where not everyone believes that access to health care is a human right; not everyone believes that access to housing is a human right; not everyone believes that housing is health care. And I think that those three things are linked together and are some of the important ingredients to have when closing the hospital to homelessness pipeline,” Keller says.
Despite the significant need for medical respite programs across the country, their future growth faces significant barriers. There is a lack of dedicated funding sources for these programs in many states, which can hinder the ability of service providers to expand into medical respite care. On top of that, there are gaps between health care and housing systems that often allow homeless people with injuries and illnesses to slip through the cracks.
How medical respite programs work
In the US, the first medical respite care programs were established in the 1980s, according to NIMRC, but most of the model’s growth occurred after 2011, when uniform standards for this type of care were established.
The programs vary widely in size, scope, and funding structure. NIMRC found that medical respite shelters have a median bed capacity of 16 — although at least one has a capacity of as many as 200-plus beds — and most limit their guests’ stay to 45 days. These programs offer short-term medical care, and they often provide guests daily meals, transportation to medical appointments and access to a phone.
More than half of medical respite programs receive funding from hospitals, which over the years have faced a staggering increase in uncompensated care. Since 2000, hospitals have provided about $745 billion in health care that has not been paid for by a patient or insurance provider, according to the American Hospital Association. People experiencing homelessness who seek treatment without Medicaid or Medicare coverage usually fall into this bucket.
Funding for medical respite programs also comes from a mixture of state governments, foundations and private donors.
Weighed down by negative news?
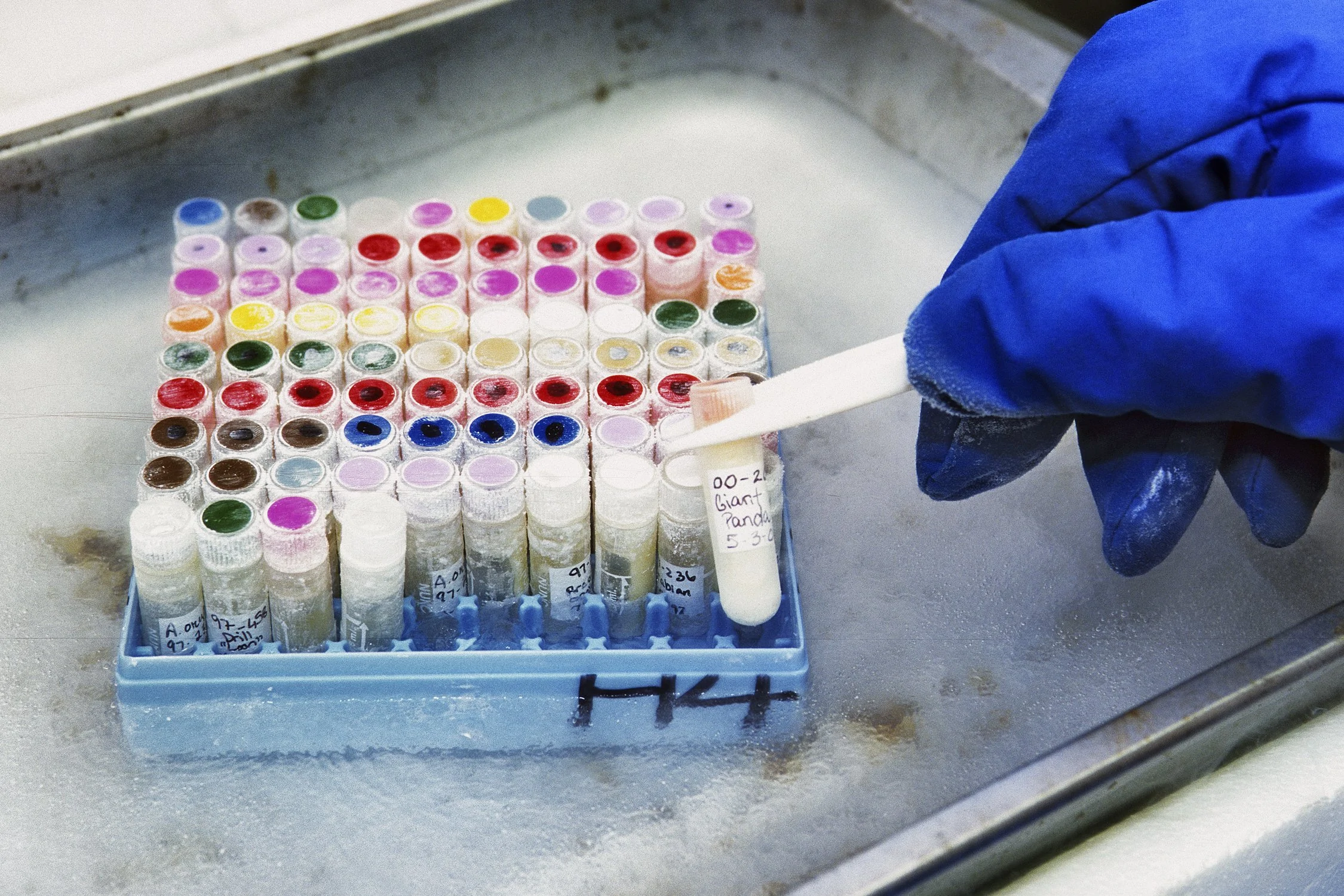
Our smart, bright, weekly newsletter is the uplift you’ve been looking for.On a broad level, these programs address some basic issues that people experiencing homelessness face, says Caitlin Synovec, NIMRC’s assistant director. For example, they give people with injuries and illnesses a private place to be treated outside a doctor’s office or hospital. They also provide a safe place to store medicines that need refrigeration, like insulin and Amoxicillin.
“Even if someone who’s experiencing homelessness is staying in a congregate shelter, or even a semi-congregate shelter, a lot of those resources aren’t available to them because there are limitations,” Synovec says.
Some medical respite care programs connect unhoused people with primary care physicians, and others provide a pathway out of homelessness through rapid rehousing programs.
RecoveryWorks, a nonprofit in Lakewood, Colorado, does it all. The first-of-its-kind shelter in Jefferson County offers case management, year-round shelter and rehousing options, and medical respite services.

James Ginsburg, RecoveryWorks’ executive director, says local homeless service providers routinely encounter people with frostbite, gangrene or open wounds. Those who receive treatment from a doctor and require additional care can be referred to RecoveryWorks, where they can stay in a medical respite bed for up to 30 days, though Ginsburg says he has extended the welcome for people with long treatment courses.
RecoveryWorks has 11 respite beds and serves between 50 and 60 people annually with medical respite care, Ginsburg added.
RecoveryWorks also has a primary care services program that connects unhoused people to primary care doctors. It partnered with STRIDE Community Health Center, a nonprofit headquartered in nearby Wheat Ridge, to provide primary care services for unhoused people. Ginsburg says the relationship with a primary care physician is often overlooked by people who are forced to live on the streets.
“Primary care is a critical component of the full recovery from homelessness,” Ginsburg says. “If you have chronic and acute care issues that are being untreated, it just makes getting housed and staying housed that much more difficult. So, this is sort of an unknown gap in the system.”
RecoveryWorks has been expanding its capacity with the recent purchase of a 34-unit motel and construction of a 700-bed shelter. “We’re really trying to collaborate with the current service providers in Jefferson County but also build out a more robust rehousing infrastructure,” Ginsburg says.
Barriers to scale
Despite the growth of medical respite programs in the US, several barriers prevent the model from becoming widely established. For instance, there is no dedicated funding source for these programs, either at the federal or state level. Any local funding that exists must usually be squeezed out of a different funding priority, like health care or homeless services, Ginsburg says. This means that facilities like RecoveryWorks must apply for funding in each budget cycle.
In Colorado, respite care providers must fill out a special Home and Community-Based Service waiver for their services to be reimbursable under the state’s Medicaid program. These waivers can be used to cover adult and child care programs. However, they must be renewed with the Centers for Medicare & Medicaid Services every five years, according to the Colorado Department of Health Care Policy and Financing, which could disrupt the funding for some caregivers. Without that reimbursement, medical respite care becomes an out-of-pocket cost for service providers.
According to NIMRC’s database, RecoveryWorks is one of 46 nationwide programs that receive state funding.
NIMRC’s Synovec says funding for medical respite programs is much more difficult in states that have not expanded their Medicaid programs. That’s one reason why states like Wyoming and Kansas do not have any such programs.
Housing subsidies like housing choice vouchers also do not consider an individual’s health status, which can result in people with serious injuries and illnesses being placed in inappropriate housing units. Keller of the National Health Care for the Homeless Council says she hopes there will be greater advocacy for states to add an individual’s health status to the housing needs assessment process.
“It highlights the perverse way in which our system prioritizes people for housing and does not integrate health needs into the assessments of individuals.”